A surgeon performs a complete bilateral mastectomy with insertion of breast prosthesis at the same surgical session.
What CPT@ coding is reported?
A physician sees a patient for the first observation visit, spends 85 minutes, with moderate MDM.
What CPT® code is reported?
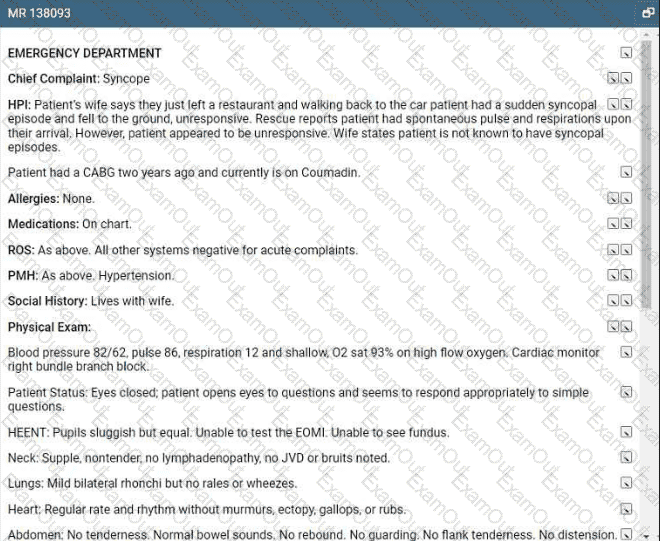
Refer to the supplemental information when answering this question:
View MR 138093
What E/M coding is reported?
A 67-year-old male presents with DJD and spondylolisthesis at L4-L5 The patient is placed prone on the operating table and, after induction of general anesthesia, the lower back is sterilely prepped and draped. One incision was made over L1-L5. This was confirmed with a probe under fluoroscopy. Laminectomies are done at vertebral segments L4 and L5 with facetectomies to relieve pressure to the nerve roots. Allograft was packed in the gutters from L1-L5 for a posterior arthrodesis. Pedicle screws were placed at L2, L3, and L4. The construct was copiously irrigated and muscle; fascia and skin were closed in layers.
Select the procedure codes for this scenario.
View MR 006399
MR 006399
Operative Report
Preoperative Diagnosis: Chronic otitis media in the right ear
Postoperative Diagnosis: Chronic otitis media in the right ear
Procedure: Eustachian tube inflation
Anesthesia: General
Blood Loss: Minimal
Findings: Serous mucoid fluid
Complications: None
Indications: The patient is a 2-year-old who presented to the office with chronic otitis media refractory to medical management. The treatment will be eustachian tube inflation to remove the fluid. Risks, benefits, and alternatives were reviewed with the family, which include general anesthetic, bleeding, infection, tympanic membrane perforation, routine tubes, and need for additional surgery. The family understood these risks and signed the appropriate consent form.
Procedure in Detail: After the patient was properly identified, he was brought into the operating room and placed supine. The patient was prepped and draped in the usual fashion. General anesthesia was administered via inhalation mask, and after adequate sedation was achieved, a medium-sized speculum was placed in the right ear and cerumen was removed atraumatically using instrument with operative microscope. The tube is dilated, an incision is made to the tympanum and thick mucoid fluid was suctioned. The patient was awakened after having tolerated the procedure well and taken to the recovery room in stable condition.
What CPT® coding is reported for this case?
A patient presents to the pulmonologist's office for the first time with coughing and shortness of breath. The patient has a history of asthma. The physician performs a medically appropriate
history and exam. The following labs are ordered: CBC, arterial blood gas, and sputum culture. The pulmonologist assesses the patient with a new diagnosis of COPD. The patient is given a
prescription for the inhaler Breo Ellipta.
What E/M code is reported?
What does the suffix -graph mean?
A patient has swelling in both arms and lymphangitis is suspected. She is in the outpatient radiology department for a lymphangiography of both arms.
What CPT® coding is correct?
A patient with compression fractures of L5 and the sacrum undergoes vertebroplasty, with cement injected into two vertebral bodies, performed bilaterally.
What CPT® coding is reported?
A patient arrives at the clinic experiencing pain due to a chest injury caused by blunt force. The provider takes X-ray imaging with 6 views of the chest.
What CPT® coding is reported?

