A healthy long-term employee with a history of Bacillus Calmette–Guérin (BCG) vaccination has a Tuberculin Skin Test (TST) result of 7 mm induration. The current Centers for Disease Control and Prevention (CDC) recommendations include which of the following?
Send the employee for a chest x-ray
No further action is required
Repeat the test in 1 to 3 weeks
Refer the employee to a physician for treatment
The Answer Is:
BExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) aligns with CDC guidance regarding interpretation of the tuberculin skin test (TST) in healthcare personnel. For a healthy individual with no known risk factors for tuberculosis, a TST is considered positive only when induration is ≥10 mm. In this scenario, the employee’s TST result of 7 mm induration is negative and does not meet the threshold for latent TB infection.
A prior history of BCG vaccination does not change interpretation criteria in adults. The CDC explicitly recommends that TST results be interpreted regardless of BCG history, as vaccine-related reactivity typically wanes over time and induration should not be attributed to BCG alone. Therefore, a 7 mm reaction in a low-risk, asymptomatic healthcare worker does not require further diagnostic evaluation.
Option A (chest x-ray) is reserved for individuals with a positive TB test or symptoms suggestive of active TB. Option C (repeat testing) is not indicated unless this was part of a two-step baseline test and the first result was negative in a newly hired employee, which is not the case here. Option D is inappropriate because treatment is only considered after confirmed latent TB infection.
For the CIC® exam, it is essential to recognize that no further action is required when TST induration is below the positive threshold for the individual’s risk category, even in those with prior BCG vaccination.
Which of the following stains is used to identify mycobacteria?
Acid-fast
Gram
Methylene blue
India ink
The Answer Is:
AExplanation:
Mycobacteria, including species such as Mycobacterium tuberculosis and Mycobacterium leprae, are a group of bacteria known for their unique cell wall composition, which contains a high amount of lipid-rich mycolic acids. This characteristic makes them resistant to conventional staining methods and necessitates the use of specialized techniques for identification. The acid-fast stain is the standard method for identifying mycobacteria in clinical and laboratory settings. This staining technique, developed by Ziehl-Neelsen, involves the use of carbol fuchsin, which penetrates the lipid-rich cell wall of mycobacteria. After staining, the sample is treated with acid-alcohol, which decolorizes non-acid-fast organisms, while mycobacteria retain the red color due to their resistance to decolorization—hence the term "acid-fast." This property allows infection preventionists and microbiologists to distinguish mycobacteria from other bacteria under a microscope.
Option B, the Gram stain, is a common differential staining technique used to classify most bacteria into Gram-positive or Gram-negative based on the structure of their cell walls. However, mycobacteria do not stain reliably with the Gram method due to their thick, waxy cell walls, rendering it ineffective for their identification. Option C, methylene blue, is a simple stain used to observe bacterial morphology or as a counterstain in other techniques (e.g., Gram staining), but it lacks the specificity to identify mycobacteria. Option D, India ink, is used primarily to detect encapsulated organisms such as Cryptococcus neoformans by creating a negative staining effect around the capsule, and it is not suitable for mycobacteria.
The CBIC’s "Identification of Infectious Disease Processes" domain underscores the importance of accurate diagnostic methods in infection control, including the use of appropriate staining techniques to identify pathogens like mycobacteria. The acid-fast stain is specifically recommended by the CDC and WHO for the initial detection of mycobacterial infections, such as tuberculosis, in clinical specimens (CDC, Laboratory Identification of Mycobacteria, 2008). This aligns with the CBIC Practice Analysis (2022), which emphasizes the role of laboratory diagnostics in supporting infection prevention strategies.
A patient with a non-crusted rash has boon diagnosed with Sarcoptes scabiei. The patient is treated with 5% permethrin and precautions are started. The precautions can be stopped
when the treatment cream is applied
when the bed linen is changed
24 hours after effective treatment
24 hours after the second treatment
The Answer Is:
CExplanation:
For Sarcoptes scabiei (scabies), Contact Precautions should remain in place until 24 hours after effective treatment has been completed. The first-line treatment is 5% permethrin cream, which is applied to the entire body and left on for 8–14 hours before being washed off.
Why the Other Options Are Incorrect?
A. When the treatment cream is applied – The mite is still present and infectious until treatment has fully taken effect.
B. When the bed linen is changed – While changing linens is necessary, it does not indicate that the infestation has cleared.
D. 24 hours after the second treatment – Most cases require only one treatment with permethrin, though severe cases may need a second dose after a week.
CBIC Infection Control Reference
According to APIC guidelines, Contact Precautions can be discontinued 24 hours after effective treatment has been administered.
Which humoral antibody indicates previous infection and assists in protecting tissue?
IgA
IgD
IgG
IgM
The Answer Is:
CExplanation:
Humoral antibodies, or immunoglobulins, play distinct roles in the immune system, and their presence or levels can provide insights into infection history and ongoing immune protection. The Certification Board of Infection Control and Epidemiology (CBIC) recognizes the importance of understanding immunological responses in the "Identification of Infectious Disease Processes" domain, which is critical for infection preventionists to interpret diagnostic data and guide patient care. The question focuses on identifying the antibody that indicates a previous infection and assists in protecting tissue, requiring an evaluation of the functions and kinetics of the five major immunoglobulin classes (IgA, IgD, IgG, IgM, IgE).
Option C, IgG, is the correct answer. IgG is the most abundant antibody in serum, accounting for approximately 75-80% of total immunoglobulins, and is the primary antibody involved in long-term immunity. It appears in significant levels after an initial infection, typically rising during the convalescent phase (weeks to months after exposure) and persisting for years, serving as a marker of previous infection. IgG provides protection by neutralizing pathogens, opsonizing them for phagocytosis, and activating the complement system, which helps protect tissues from further damage. The Centers for Disease Control and Prevention (CDC) and clinical immunology references, such as the "Manual of Clinical Microbiology" (ASM Press), note that IgG seroconversion or elevated IgG titers are commonly used to diagnose past infections (e.g., measles, hepatitis) and indicate lasting immunity. Its ability to cross the placenta also aids in protecting fetal tissues, reinforcing its protective role.
Option A, IgA, is primarily found in mucosal secretions (e.g., saliva, tears, breast milk) and plays a key role in mucosal immunity, preventing pathogen adhesion to epithelial surfaces. While IgA can indicate previous mucosal infections and offers localized tissue protection, it is not the primary systemic marker of past infection or long-term tissue protection, making it less fitting. Option B, IgD, is present in low concentrations and is mainly involved in B-cell activation and maturation, with no significant role in indicating previous infection or protecting tissues. Option D, IgM, is the first antibody produced during an acute infection, appearing early in the immune response (within days) and indicating current or recent infection. However, its levels decline rapidly, and it does not persist to mark previous infection or provide long-term tissue protection, unlike IgG.
The CBIC Practice Analysis (2022) and CDC guidelines on serological testing emphasize IgG’s role in assessing past immunity, supported by immunological literature (e.g., Janeway’s Immunobiology, 9th Edition). Thus, IgG is the humoral antibody that best indicates previous infection and assists in protecting tissue, making Option C the correct choice.
Which of the following is an example of a syndromic surveillance indicator?
Number of individuals presenting with influenza-like illness in the emergency department each day
Number of individuals presenting with laboratory-confirmed influenza in the emergency department each day
Rate of central line–associated bloodstream infections each quarter
Number of cases of methicillin-resistant Staphylococcus aureus in an intensive care unit each month
The Answer Is:
AExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) describes syndromic surveillance as a surveillance method that focuses on clinical signs, symptoms, or health-seeking behaviors rather than confirmed diagnoses. Its primary purpose is early detection of outbreaks or emerging health threats, often before laboratory confirmation is available.
Option A is the correct example because tracking the number of individuals presenting with influenza-like illness (ILI) relies on symptom patterns such as fever, cough, and sore throat. These data are typically collected in near real time from emergency department chief complaints or triage notes, allowing infection preventionists and public health authorities to identify unusual increases quickly and initiate early response measures.
Option B is not syndromic surveillance because it depends on laboratory-confirmed diagnoses, which are characteristic of traditional, diagnosis-based surveillance. Option C represents device-associated infection surveillance, which is retrospective and outcome-focused. Option D involves laboratory-confirmed antimicrobial-resistant organisms and is also not syndromic.
For CIC® exam preparation, it is important to remember that syndromic surveillance prioritizes speed over diagnostic certainty. By monitoring symptom clusters rather than confirmed cases, it enables earlier recognition of outbreaks such as influenza, gastrointestinal illness, or bioterrorism-related events, making it a critical component of public health preparedness and response.
What rate is expressed by the number of patients who acquire infections over a specified time period divided by the population at risk of acquiring an infection during that time period?
Incidence rate
Disease specific
Point prevalence
Period prevalence
The Answer Is:
AExplanation:
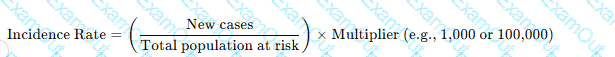
The incidence rate measures new cases of infection in a population over a defined time period using the formula:
Why the Other Options Are Incorrect?
B. Disease specific – Refers to infections caused by a particular pathogen, not the general rate of new infections.
C. Point prevalence – Measures existing cases at a specific point in time, not new cases.
D. Period prevalence – Includes both old and new cases over a set period, unlike incidence, which only considers new cases.
CBIC Infection Control Reference
APIC defines incidence rate as the number of new infections in a population over a given period.
The intensive care unit has noted an increase in patients with ventilator-associated events (VAEs). Which of the following may be contributing to the increase in these events?
Supine position during transport
Daily sedation vacation
Daily weaning assessment
Daily oral care with chlorhexidine
The Answer Is:
AExplanation:
Ventilator-associated events (VAEs) are complications that occur in patients receiving mechanical ventilation and include conditions such as ventilator-associated pneumonia (VAP), pulmonary edema, and atelectasis. The CBIC Certified Infection Control Exam Study Guide (6th edition) emphasizes that patient positioning plays a critical role in preventing aspiration and subsequent respiratory complications in mechanically ventilated patients.
Maintaining patients in a supine position, particularly during transport, increases the risk of aspiration of gastric contents and oropharyngeal secretions. Aspiration is a well-recognized contributing factor to the development of VAEs because it can lead to infection, inflammation, and worsening oxygenation. The Study Guide recommends maintaining the head of the bed elevated (generally 30–45 degrees) whenever feasible, including during care activities and transport, to reduce aspiration risk.
The other options listed—daily sedation vacation, daily weaning assessment, and daily oral care with chlorhexidine—are evidence-based prevention strategies that are part of ventilator care bundles. These interventions are designed to reduce the duration of mechanical ventilation, improve pulmonary function, and decrease microbial colonization, all of which lower the risk of VAEs rather than contribute to them.
Therefore, supine positioning during transport is the most likely factor contributing to an increase in ventilator-associated events and represents a deviation from recommended infection prevention practices.
During the past week, three out of four blood cultures from a febrile neonate in an intensive care unit grew coagulase-negative staphylococci. This MOST likely indicates:
Laboratory error.
Contamination.
Colonization.
Infection.
The Answer Is:
BExplanation:
The scenario involves a febrile neonate in an intensive care unit (ICU) with three out of four blood cultures growing coagulase-negative staphylococci (CoNS) over the past week. The Certification Board of Infection Control and Epidemiology (CBIC) emphasizes accurate interpretation of microbiological data in the "Identification of Infectious Disease Processes" domain, aligning with the Centers for Disease Control and Prevention (CDC) guidelines for healthcare-associated infections. Determining whether this represents a true infection, contamination, colonization, or laboratory error requires evaluating the clinical and microbiological context.
Option B, "Contamination," is the most likely indication. Coagulase-negative staphylococci, such as Staphylococcus epidermidis, are common skin flora and frequent contaminants in blood cultures, especially in neonates where skin preparation or sampling technique may be challenging. The CDC’s "Guidelines for the Prevention of Intravascular Catheter-Related Infections" (2017) and the Clinical and Laboratory Standards Institute (CLSI) note that multiple positive cultures (e.g., two or more) are typically required to confirm true bacteremia, particularly with CoNS, unless accompanied by clear clinical signs of infection (e.g., worsening fever, hemodynamic instability) and no other explanation. The inconsistency (three out of four cultures) and the neonate’s ICU setting—where contamination from skin or catheter hubs is common—suggest that the positive cultures likely result from contamination during blood draw rather than true infection. Studies, such as those in the Journal of Clinical Microbiology (e.g., Beekmann et al., 2005), indicate that CoNS in blood cultures is contaminated in 70-80% of cases when not supported by robust clinical correlation.
Option A, "Laboratory error," is possible but less likely as the primary explanation. Laboratory errors (e.g., mislabeling or processing mistakes) could occur, but the repeated growth in three of four cultures suggests a consistent finding rather than a random error, making contamination a more plausible cause. Option C, "Colonization," refers to the presence of microorganisms on or in the body without invasion or immune response. While CoNS can colonize the skin or catheter sites, colonization does not typically result in positive blood cultures unless there is an invasive process, which is not supported by the data here. Option D, "Infection," is the least likely without additional evidence. True CoNS bloodstream infections (e.g., catheter-related) in neonates are serious but require consistent positive cultures, clinical deterioration (e.g., persistent fever, leukocytosis), and often imaging or catheter removal confirmation. The febrile state alone, with inconsistent culture results, does not meet the CDC’s criteria for diagnosing infection (e.g., at least two positive cultures from separate draws).
The CBIC Practice Analysis (2022) and CDC guidelines stress differentiating contamination from infection to avoid unnecessary treatment, which can drive antibiotic resistance. Given the high likelihood of contamination with CoNS in this context, Option B is the most accurate answer.
Which of the following findings indicates that a sputum sample has been properly collected from a patient with possible bacterial pneumonia?
Numerous neutrophils and few, if any, epithelial cells.
Presence of blood.
Many epithelial cells and few neutrophils.
Presence of both gram-positive and gram-negative bacteria.
The Answer Is:
AExplanation:
The CBIC Certified Infection Control Exam Study Guide (6th edition) explains that the quality of a sputum specimen is critical for accurate diagnosis of bacterial pneumonia. A properly collected sputum sample should originate from the lower respiratory tract, not from saliva or the oropharynx. Microscopic examination of the specimen—typically using a Gram stain—is used to assess specimen adequacy before culture results are interpreted.
A high-quality sputum specimen is characterized by numerous neutrophils and few or no squamous epithelial cells. Neutrophils indicate an inflammatory response in the lower airways, consistent with bacterial infection. In contrast, epithelial cells originate from the mouth and upper respiratory tract; a large number of epithelial cells suggests contamination with saliva and an improperly collected specimen.
Option A correctly describes these criteria and therefore indicates proper specimen collection. Option C reflects poor-quality sputum contaminated with oral secretions and should be rejected or recollected. Option B (presence of blood) may occur in pneumonia but does not indicate specimen quality. Option D is nonspecific and may represent contamination or colonizing flora rather than true infection.
For the CIC® exam, it is important to recognize that specimen validity precedes interpretation of microbiologic results. The presence of abundant neutrophils with minimal epithelial cells confirms that the sputum sample is appropriate for diagnosing bacterial pneumonia and supports accurate clinical and epidemiologic decision-making.
Which of the following operating suite design features is LEAST important for the prevention of infection?
Type of floor material
Positive pressure air handling
Placement of sinks for surgical scrubs
Control of traffic and traffic flow patterns
The Answer Is:
AExplanation:
The correct answer is A, "Type of floor material," as it is the least important operating suite design feature for the prevention of infection compared to the other options. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, the design of operating suites plays a critical role in infection prevention, particularly for surgical site infections (SSIs). While the type of floor material (e.g., vinyl, tile, or epoxy) can affect ease of cleaning and durability, its impact on infection prevention is secondary to other design elements that directly influence air quality, hygiene practices, and personnel movement (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.5 - Evaluate the environment for infection risks). Modern flooring materials are generally designed to be non-porous and easily disinfected, mitigating their role as a primary infection risk factor when proper cleaning protocols are followed.
Option B (positive pressure air handling) is highly important because it prevents the influx of contaminated air into the operating suite, reducing the risk of airborne pathogens, including those causing SSIs. This is a standard feature in operating rooms to maintain a sterile environment (AORN Guidelines for Perioperative Practice, 2023). Option C (placement of sinks for surgical scrubs) is critical for ensuring that surgical staff can perform effective hand and forearm antisepsis, a key step in preventing SSIs by reducing microbial load before surgery. Option D (control of traffic and traffic flow patterns) is essential to minimize the introduction of contaminants from outside the operating suite, as excessive or uncontrolled movement can increase the risk of airborne and contact transmission (CDC Guidelines for Environmental Infection Control in Healthcare Facilities, 2019).
The relative unimportance of floor material type stems from the fact that infection prevention relies more on consistent cleaning practices and the aforementioned design features, which directly address pathogen transmission routes. This aligns with CBIC’s focus on evaluating environmental risks based on their direct impact on infection control (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.4 - Implement environmental cleaning and disinfection protocols).

